Clinical Laser Patient FAQs
Laser-Assisted Hatching FAQ
Q: What is assisted hatching?
A: In order for an embryo to implant in the uterine lining, the inner embryo (blastocyst) must “hatch” from its protective outer shell (the zona pellucida). Assisted hatching is a technique in which the zona pellucida of an embryo is purposely weakened or cut to help the embryo hatch more easily and promote implantation.
Q: What are the different ways of performing assisted hatching?
A: There are three methods of assisted hatching: mechanical, chemical, and laser-assisted. With mechanical methods, an incision or hole is made in the zona pellucida using a tool such as a microsurgical knife or a special glass needle. The chemical method directs a stream of acidic hatching solution against outer shell to digest a portion of the zona pellucida. Laser-assisted hatching (LAH) uses a highly focused laser beam to remove the zona pellucida in very precise increments.
Q: Who should have assisted hatching of their embryos?
A: The most commonly used indications for use of assisted hatching are:
| Age | Women over 37 years old |
| Hormonal Status | Women with an elevated baseline level of FSH (follicular stimulating hormone) |
| Embryo Quality | Women with poor prognosis embryos, including conditions such as a thick zona pellucida, slow cell division rate, or high cell fragmentation |
| IVF Attempts | Women who have failed 1 or more IVF cycles |
| Frozen Embryos | Women using frozen/thawed embryos, which may have hardened zona pellucida |
Q: What are the risks of assisted hatching using the laser?
A: The risks of assisting hatching using the laser are similar to the risks when using chemical or mechanical methods. These risks include possible damage / destruction to the embryo and a possible increased chance of monozygotic (identical) twinning.
Q: What are the benefits of assisted hatching using the laser?
A: Laser-assisted hatching may require less embryo handling than other assisted hatching methods. Also, laser-assisted hatching may be faster than other methods and therefore the embryo may spend less time outside of the incubator.
Q: What do we know about the health of babies born following laser-assisted hatching?
A: In recent follow-up studies of babies born after laser-assisted hatching, no increase in major or minor congenital abnormalities and no observable changes in the cells’ genetic material were noted.
Embryo Biopsy FAQ
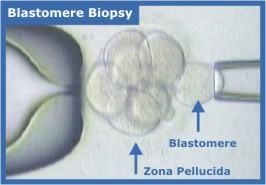
Q: What is blastomere biopsy?
A: Blastomere biopsy is one method used for embryo biopsy. When an embryo reaches the third day of development, it normally has eight cells. One or two of these cells, called “blastomeres,” can be removed from the embryo. The embryo can go on to develop just as though the one cell or two cells were never removed.
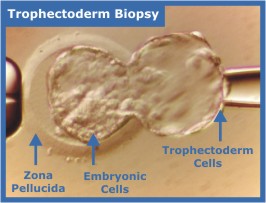
Q: What is trophectoderm biopsy?
A: Trophectoderm biopsy is another method used for embryo biopsy. Trophectoderm cells are extra-embryonic tissue; this means that it does not become part of the fetus but becomes part of supporting structures, such as the placenta and membranes. Trophectoderm biopsy takes place at the 16-32 cell “blastocyst” stage of development, as the trophectoderm is beginning to herniate through the zona pellucida. Instead of removing individual blastomeres, several trophectoderm cells are removed.
Q: Why is embryo biopsy performed?
A: The cells removed during the biopsy procedure are used to perform pre-implantation genetic diagnosis (PGD), which shows the chromosomal composition of the embryos, and if they carry a specific disease-producing mutation. One or more embryos free of conditions that would cause serious disease may then be implanted in a woman’s uterus.
Q: What are the different ways of performing the embryo biopsy procedures?
A: There are three methods of biopsy procedures: mechanical, chemical, and laser zona drilling. With mechanical methods, an incision or hole is made in the zona pellucida (the outer layer) using a tool such as a microsurgical knife or a special glass needle. The chemical method directs a stream of acidic solution to digest a portion of the zona pellucida. Laser zona drilling uses a highly focused laser beam to remove the zona pellucida in very precise increments.
Q: How is the laser used during the embryo biopsy procedures?
A: For blastomere biopsy, the laser is used to drill an opening in the zona pellucida to facilitate insertion of the pipet used to remove the blastomere. For trophectoderm biopsy, the laser is first used to create an opening in the zona to promote herniation of the trophectoderm. After the trophectoderm has protruded, the laser is also used to help separate the trophectoderm cells.
Q: What type of conditions can PGD detect?
A: To date, PGD has been most widely used to enable the birth of children free from diseases such as Down’s Syndrome, Tay-Sachs disease, Beta-thalassemia, Cystic Fibrosis, and Duchenne Muscular Dystrophy. Any gene disorder in which the DNA base pairs or code is known can be detected by PGD.
Q: What are the indications for embryo biopsy for PGD?
A: The most commonly used indications for PGD are:
- Carriers of single gene disorders.
These patients benefit from PGD by reducing the risk of conceiving an affected baby. - Recurrent Miscarriage
Fertile couples with repeated miscarriages should be evaluated for the presence of a chromosomal abnormality. The female or male partner may be a carrier of a balanced translocation or be an aneuploid mosaic. - Unsuccessful IVF cycles
Couples with repeated unsuccessful IVF cycles should be evaluated for the presence of a chromosome abnormality. The female or male partner may be a carrier of a balanced translocation or be an aneuploid mosaic. - Unexplained Infertility
The most probable cause of unexplained infertility or history of habitual miscarriage is a chromosome abnormality. The male OR female partner may be a carrier of a translocation or be an aneuploid mosaic. - Aneuploidy and Advanced Maternal Age
Women of advanced maternal age (> 35) are at a higher risk of producing aneuploid embryos, resulting in implantation failure, a higher risk of miscarriage or the birth of a child with a chromosome abnormality (e.g. Down syndrome).
Q: What are the risks of embryo biopsy using the laser?
A: The risks of embryo biopsy using the laser are similar to the risks when using chemical or mechanical methods. These risks include possible damage / destruction to the embryo and a possible increased chance of monozygotic (identical) twinning.
Q: What are the benefits of embryo biopsy using the laser?
A: Using the laser for embryo biopsy requires less embryo handling, allows for more precision and control, is less traumatic, and reduces technician variation as compared to chemical and mechanical methods. Because laser embryo biopsy is faster than the other methods, the embryo spends less time outside the incubator and is less likely to be harmed.
